A research team led by the University of Oregon’s Nicole Swann has zeroed in on what may be easily detectable markers of Parkinson’s disease.
The evidence is in the specific angles and sharpness of electrical waves in unfiltered raw data captured by scalp electroencephalograms of patients receiving treatment for the degenerative disease that slowly damages the central nervous system.
Noninvasive scalp EEG, in which electrodes briefly placed on the head measure brain waves, is used at medical facilities around the world and is a relatively inexpensive technology. Harnessing it, Swann said, could aid in both the diagnosis of Parkinson’s disease and fine-tune therapeutic treatments for it and other motor disorders.
“Using this safe and affordable way to measure and quantify brain activity, we were able to distinguish differences between Parkinson’s patients who were on and off medications and in comparisons with healthy people,” said Swann, a professor in the Department of Human Physiology.
Swann, along with colleagues from the University of California San Diego, reported the findings in a paper on the characteristics of waveform shape in Parkinson's disease in the May 20 issue of the free-access online journal eNeuro. The journal is a sister publication of the high-profile Journal of Neuroscience.
In 2017, Scott Cole, a co-author of the new study and then a doctoral student at UC San Diego, had noticed that Parkinson's patients appeared to have sharp brain waves in invasive brain recordings acquired during neurosurgery, suggesting a new look was warranted.
The new study, Swann said, showed that similar patterns are evident in scalp EEG recordings – an affordable and safe method which can be used on anyone – extending the translational power of the previous work.
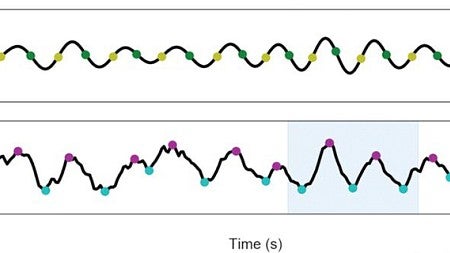
Previous efforts to detect Parkinson’s disease with EEG have been inconsistent, she said, because researchers have modeled brain signals as sine waves, which are beta waves filtered to round the waves and show the overall power of periodic oscillations. The current work uses a new analytic approach.
Nick Jackson, a lab technician in the Swann lab who is now pursuing a doctoral degree at the University of Texas at Austin, was first author of the new paper.
“The raw signals go up and down like sine waves but with more asymmetry,” Swann said. “The steepness – the slant – turns out to be important in Parkinson’s patients. This was easily detectable in the patients who are off medication.”
When the peak is sharper at the top of the wave than in the trough, or low part of the oscillation, it is indicative of patients who are off their medications, she said.
The initial diagnosis of Parkinson’s disease now relies on a neurologist’s assessment of patients as they complete a series of body-movement tasks. Such subjective testing, however, can lead to misdiagnosis.
“We don’t know yet whether this approach will be better, but it could provide easily obtained brain measurements that would be helpful and possibly used in tandem with clinical observations and other EEG measurements,” Swann said.
Current treatments for Parkinson’s disease involve surgery to permanently implant an electric stimulator and/or a drug-based approach where finding the best dosage is difficult and often results in frustrating cycling of effectiveness, said co-author Bradley Voytek, a neuroscientist at UC San Diego.
In a large follow-up study soon to be done at the UO, Swann said she hopes to combine scalp EEG measurements with detailed medical histories of patients, along with self-reports of how each person is feeling on testing days. Eventually, it is hoped the approach could help detect changes in the disease in individuals over time.
Finding such measures of the course of the disease in real time, Voytek said, could lead to quick treatment adjustments.
“In the case of an invasive brain stimulator, this might mean only applying electric stimulation when it's needed,” he said. “In the case of pharmacology, it would mean adjusting a drug's dose much like continuous glucose monitoring done by an implant can signal a pump to adjust insulin levels as needed.”
Ideally, Swann said, if the approach proves to provide robust information, EEG testing could be remotely done by Parkinson’s patients wearing a hat fitted with electrodes. The data could then be sent to their doctor, helping to avoid frequent trips to a neurologist for patients for whom travel may be a barrier to treatment.
—By Jim Barlow, University Communications


