Parasitic worms that go from the soil into humans and pet hosts may soon receive their eviction notices thanks to progress by UO researchers.
Testing potential new drugs that target the worms, which cause serious health problems in as many as 3 billion people mostly in economically poor regions lacking adequate sanitation, is now possible through the adaption of a device invented at the UO for other research.
UO biologist Janis Weeks led the transformation under a grant awarded to her in 2013 by the Bill & Melinda Gates Foundation's Grand Challenges Explorations program. The original device was designed to study the central nervous system in small organisms, particularly the roundworm Caenorhabditis elegans.
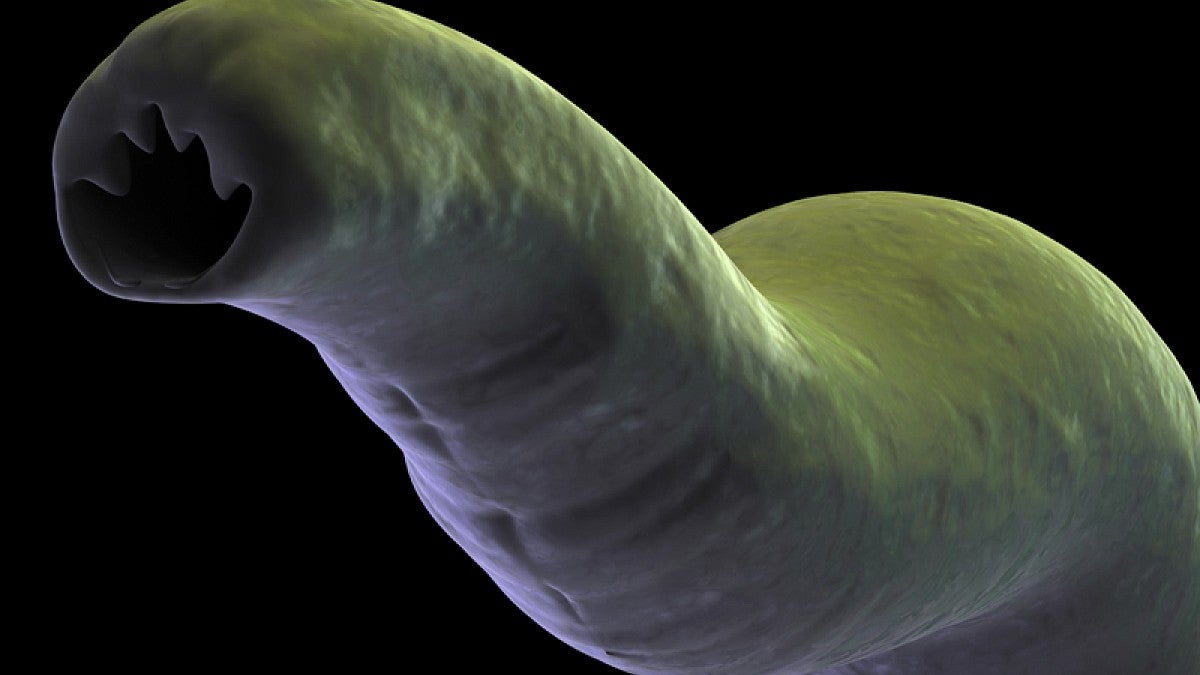
Many people carry one or all three of the common soil-transmitted worms Ascaris, whipworm and hookworm. They also infect livestock and pets.
In a new paper, Weeks and colleagues confirmed that the tiny microfluidic chip allows for the screening of potential compounds or natural products for new treatments in up to eight live parasitic worms at a time. During testing, the worms are maintained in fluids similar to the environment experienced by larvae in their infective stage.
"I've been working in Africa for 20 years teaching neuroscience," Weeks said. "I've seen the impacts of parasitic infections first-hand. I was working on C. elegans, and we had shown the connection of electrical signals to contractions in the worm's pharynx. I thought our device had possibilities for looking at parasitic worms so I developed a proposal for a Gates Foundation grant."
Her group's findings were published in December in a special issue of the International Journal for Parasitology: Drugs and Drug Resistance. Preliminary findings were presented previously at a conference in San Diego that devoted to the fight against the worms.
After contact with soil, the worms' larvae enter the body via the skin or ingestion. They thrive in the intestines, daily producing thousands of eggs. Their presence leads to such problems as anemia, malnutrition, vitamin-A deficiency, abdominal swelling, weight loss, diarrhea and intestinal inflammation. The effects are particularly damaging in children, whose physical and cognitive development can be stunted.
When the worms are in the device, electrical monitoring — similar to a human electrocardiogram — captures the signaling between neurons and muscles as the throat rhythmically pumps while feeding. When potentially disruptive compounds are injected, researchers can determine which ones disrupt the pumping to starve and eventually kill the worms.
Weeks and UO colleague Shawn Lockery, a biologist and co-author on the paper, initially developed the device for noninvasive studies of C. elegans, a widely used model organism. Four of the paper's eight co-authors own equity in NemaMetrix Inc., which now holds the commercial license for that device. The UO owns the intellectual property and has a patent pending.
"We need new drugs against these soil-transmitted parasitic infections," said Weeks, a member of the UO's Institute of Neuroscience and African Studies Program. "For most of the successful drugs that act on neurons or muscles we have had no way to assay for this property. Our device provides a really specific test for potential new drugs, and it is rapid."
There are shortcomings with therapeutics now used against infection, Weeks said. Among them is a growing threat of resistance. Each worm also requires separate drugs, which also pose health complications for pregnant women.
"All of the drugs used today to treat these infections in humans were initially discovered for use in animals," Weeks said. "We hope our new tool will help to speed the design and discovery of new drug treatments."
—By Jim Barlow, University Communications